IV Furosemide in Heart Failure: How Big is the BP Drop?
A Critical Appraisal of the Harrison et al. (2025) Paper
The Clinical Question (PICO)
Population: 253 adult patients in 5 US Emergency Departments with acute decompensated heart failure (ADHF).
Intervention: Administration of intravenous (IV) furosemide.
Comparison: The study used multivariable-adjusted mixed-effects regression to isolate the haemodynamic effect of IV furosemide from all other confounders (e.g., other treatments, baseline patient factors).
Outcome: Change in systolic blood pressure (SBP) and the risk of hypotension (defined as SBP < 90 mmHg).
Study Design
- Multicentre prospective observational cohort study.
- Recruited from 5 US EDs.
- Used continuous (beat-to-beat) BP monitoring via a finger-cuff monitor (ClearSight).
- Collected 598 person-hours of monitoring (91,210 observations).
Who Was Studied? (n=253)
Median Age: 60 years
45% female
Median Ejection Fraction: 40%
(IQR 25-59%)
Median SBP at time of IVFu: 148 mmHg
(IQR 126-174 mmHg)
Median IV Furosemide Dose: 40mg
(Analysis also covered 80mg & 100mg)
How much of the BP drop is *actually* from the furosemide?
1.4%
...of the total variance in SBP was explained by IV furosemide.
1.7%
...of the total risk of hypotension was explained by IV furosemide.
The vast majority (~98%) of BP variation was due to confounders like baseline SBP, comorbidities, and other treatments.
Magnitude of BP Drop
-11.9 mmHg
Adjusted *average* SBP drop after 80mg IV Furosemide.
~147 minutes
Time to nadir (lowest BP), with a max drop of -15.2 mmHg.
The effect was transient, with BP returning towards baseline by 6 hours.
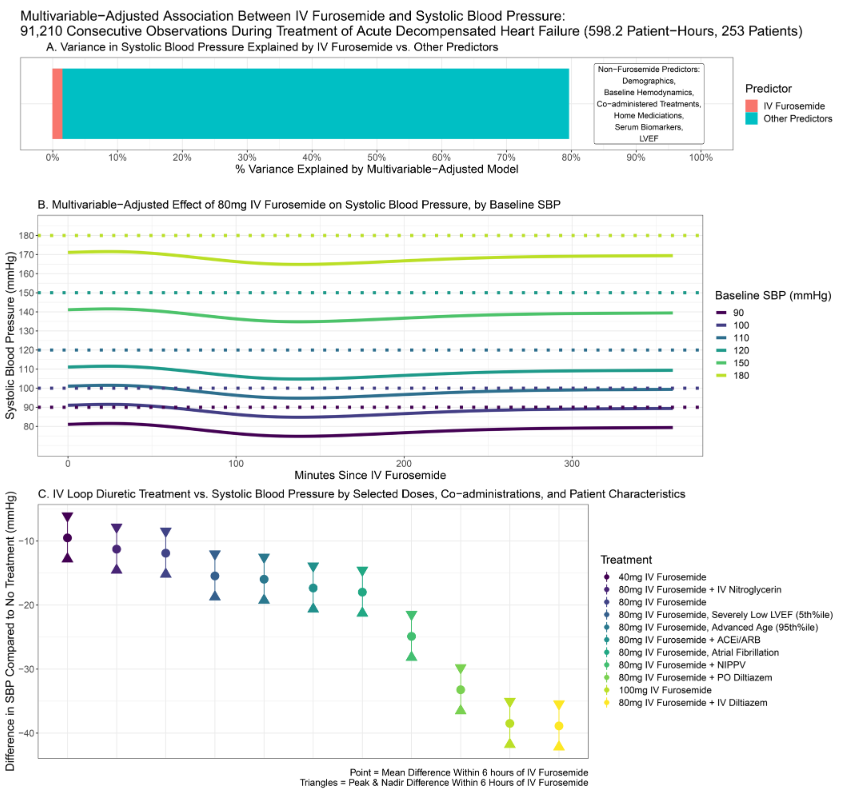
Multivariable-adjusted effect of 80mg IV Furosemide on SBP, stratified by baseline SBP. (Panel B from Figure 2)
Clinical Bottom Line
BP reductions from IV furosemide are modest, transient, and predictable.
Do not withhold guideline-directed IV furosemide in ADHF for fear of hypotension, *unless* the patient's baseline SBP is already low or they are on other high-risk vasoactive drugs.
What is the *Actual* Risk of Hypotension (SBP < 90)?
The adjusted risk was overwhelmingly dependent on baseline SBP, not just the furosemide.
For a 40mg IV Furosemide Dose:
If baseline SBP ≥ 110 mmHg:
< 1% Risk
If baseline SBP 90-100 mmHg:
≤ 2% Risk
For an 80mg IV Furosemide Dose:
If baseline SBP ≥ 120 mmHg:
≤ 2% Risk
If baseline SBP 90-100 mmHg:
3-4% Risk
No patient experienced sustained hypotension for ≥ 30 consecutive minutes.
Cumulative Minutes of Hypotension (in 6 hours)
This table (from Figure 4) shows the multivariable-adjusted cumulative minutes (95% CI) of hypotension (SBP < 90) within 6 hours of giving IV furosemide.
| Baseline SBP | 40mg Furosemide | 80mg Furosemide | 100mg Furosemide |
|---|---|---|---|
| 90 mmHg | 6 (2-10) | 14 (9-21) | 23 (16-30) |
| 100 mmHg | 4 (1-8) | 11 (6-17) | |
| 110 mmHg | 3 (1-7) | 9 (4-13) | 14 (8-20) |
| 120 mmHg | 2 (0-5) | 7 (2-11) | 10 (6-16) |
| 130 mmHg | 2 (0-4) | 5 (2-9) | 8 (4-13) |
| 150 mmHg | 1 (0-3) | 3 (0-6) | 5 (2-9) |
| 180 mmHg | 0 (0-1) | 1 (0-3) | 2 (0-5) |
Key Takeaway: Even with a low SBP of 90, a 40mg dose resulted in a median of only 6 cumulative minutes of hypotension over 6 hours. With a more typical SBP of 120, an 80mg dose resulted in only 7 minutes.
Strengths & Limitations
Strengths
- Prospective, multicentre design.
- Continuous beat-to-beat BP monitoring, which is far more accurate for this question than intermittent cuff measurements.
- Robust, modern statistical modelling (mixed-effects regression) to isolate the drug's true effect from confounders.
- Clinically relevant and pragmatic question.
Limitations
- Observational design: Cannot prove causation, only association (though it's strong).
- Finger-cuff monitoring is not the same as an arterial line (though validated to be close).
- Sample included few doses > 100mg, so results may not apply to very high-dose strategies.
- Doesn't assess repeated or "stacked" dosing, only the initial ED dose.
Further Resources
Video Summary
Podcast
Critical Appraisal Points for UK EM Practice
1. Identify the *Real* Culprits: It's the combination that matters.
This study found that IV furosemide alone has a modest effect. The real danger comes from multiplicative interactions.
The analysis showed that co-administration of furosemide with IV or PO Diltiazem, NIPPV, or ACEi/ARBs was associated with a significantly greater drop in SBP.
In practice, this means your haemodynamic caution should be exponentially higher in a patient receiving furosemide *and* one of these other therapies.
2. This Paper Should Re-frame (and reduce) Our Fear.
Many clinicians (up to 20% in one survey) admit to withholding or under-dosing IV furosemide due to fear of hypotension, even when SBP is normal.
This paper provides strong evidence that this fear is likely overstated. In the majority of ADHF patients (who present with SBP > 120 mmHg), the risk of clinically significant hypotension from a standard 40-80mg dose is minimal (<2%).
The focus should shift from "will the furosemide cause hypotension?" to "is the patient's *baseline SBP* and *comorbid medication list* safe for diuresis?"
3. This Supports Guideline-Directed Care.
We know that inadequate decongestion in hospital leads to a 3- to 6-fold increase in short-term readmission and death. Under-dosing diuretics is harmful.
This study is reassuring and empowers us to follow guidelines: for the typical hypertensive or normotensive ADHF patient, administering an appropriate dose of IV furosemide is haemodynamically safe and is the correct treatment to improve patient outcomes.